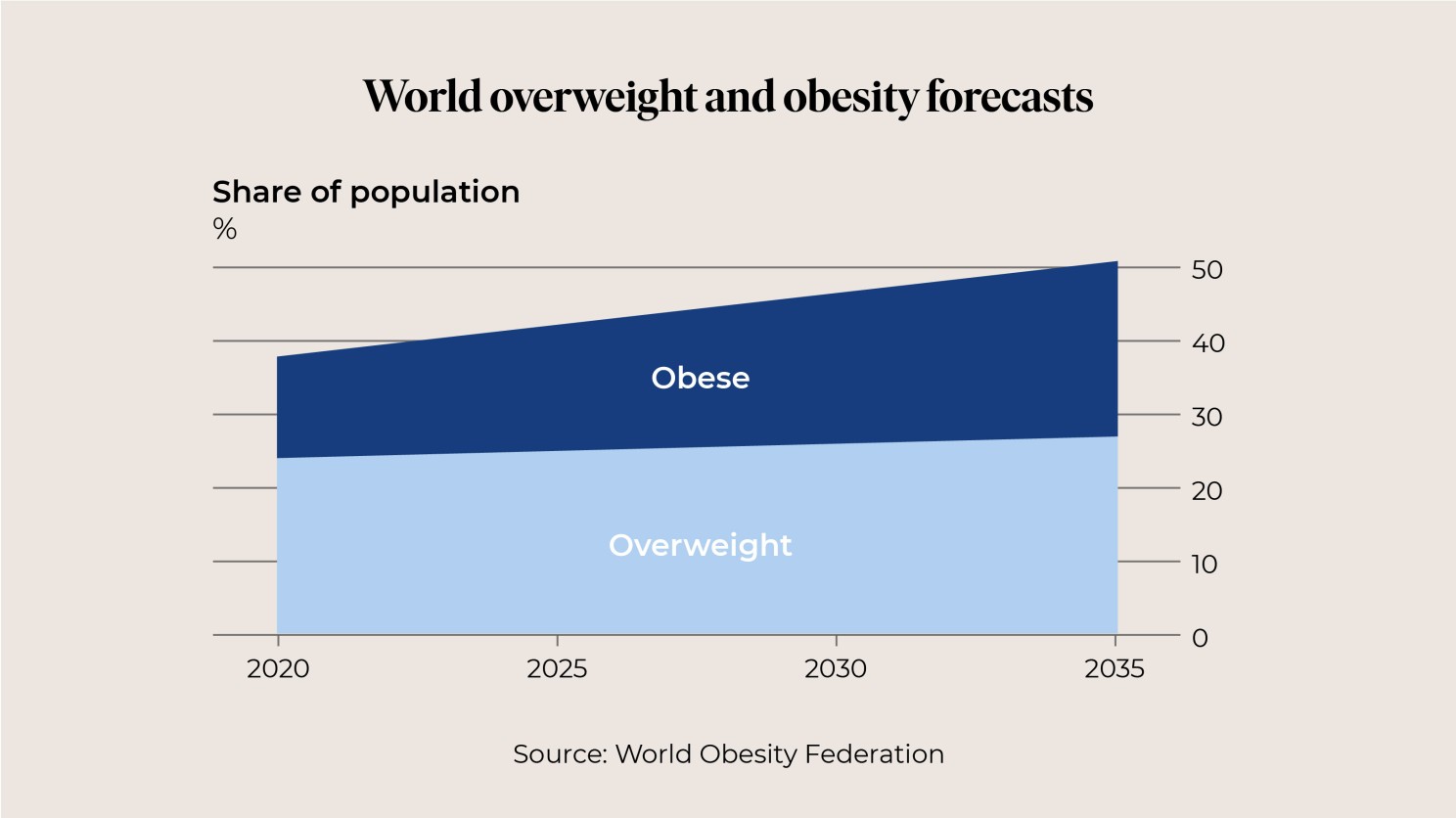
Despite the world shelling out $250 billion on weight loss products and services annually, two fifths of humanity are overweight or obese.
That’s 3.2 billion of us who are not as healthy as we could be, and by 2035, this could increase to 4 billion humans, according to the World Obesity Federation.
It’s not as if it’s just a first world problem. Developing countries are all experiencing this alarming trend.
We’re getting fatter and so far, no amount of jogging, aerobics, jazzercize, Keto, Atkins, Paleo or ‘healthy’ carb diets have been able to hold back the planet’s growing waistlines.
It’s not some sort of worldwide willpower failure either.
In fact, the issue starts at a biological level.
Humanity’s genes evolved to help our body’s maintain extra fat over winter or during famines, and they’re still fulfilling their cellular instincts.
To resist losing weight.
This, combined with the supply of super convenient, delicious, processed food is at the root of our problem.
As weight-inducing meals started hitting shelves, technology made our lifestyles increasingly more sedentary.
Growing obesity brings with it a host of other problems too, like diabetes, heart disease, high blood pressure, stroke, gout and various cancers.
While fat shaming is wrong, the stigma associated with being obese is one of the hardest to change and causes unhappiness on a tragic scale.
It’s against all these tensions that Semaglutide and other similar drugs are promising to make an amazing and effective difference.
How do they work?
The once-a-week injection acts as an appetite suppressant by behaving like a hormone called Glucagon, like peptide-1 (GLP-1).
GLP-1 is the hormone that’s released after eating to make you feel full and satisfied, Semaglutide mimics this, helping you feel full, so you don’t overeat.
The suppressant also turns off our biological, instinctive urge to eat, something that even the most determined dieters find difficult to resist.
The effect was first noticed in diabetes patients who take Ozempic.
“Ozempic which contains Semaglutide is used to treat diabetes and has been very effective for weight loss,” explains New York-based surgeon, Dr Jennifer Levine.
“It works by causing the pancreas to secrete more insulin and decreases the amount of glucagon produced by the liver, which suppresses appetite and slows down gastric motility, so you feel full for longer.”
International banking giant UBS claims it could become the biggest drug ever.
Jefferies, a US investment bank, says that by 2031 the market for these drugs could exceed US$150 billion, a figure on par with all cancer drugs combined.
Here in New Zealand, we’re not immune from feeling our clothes tighten.
In 2021, around 34.3 percent of New Zealanders were obese, our highest statistic ever.
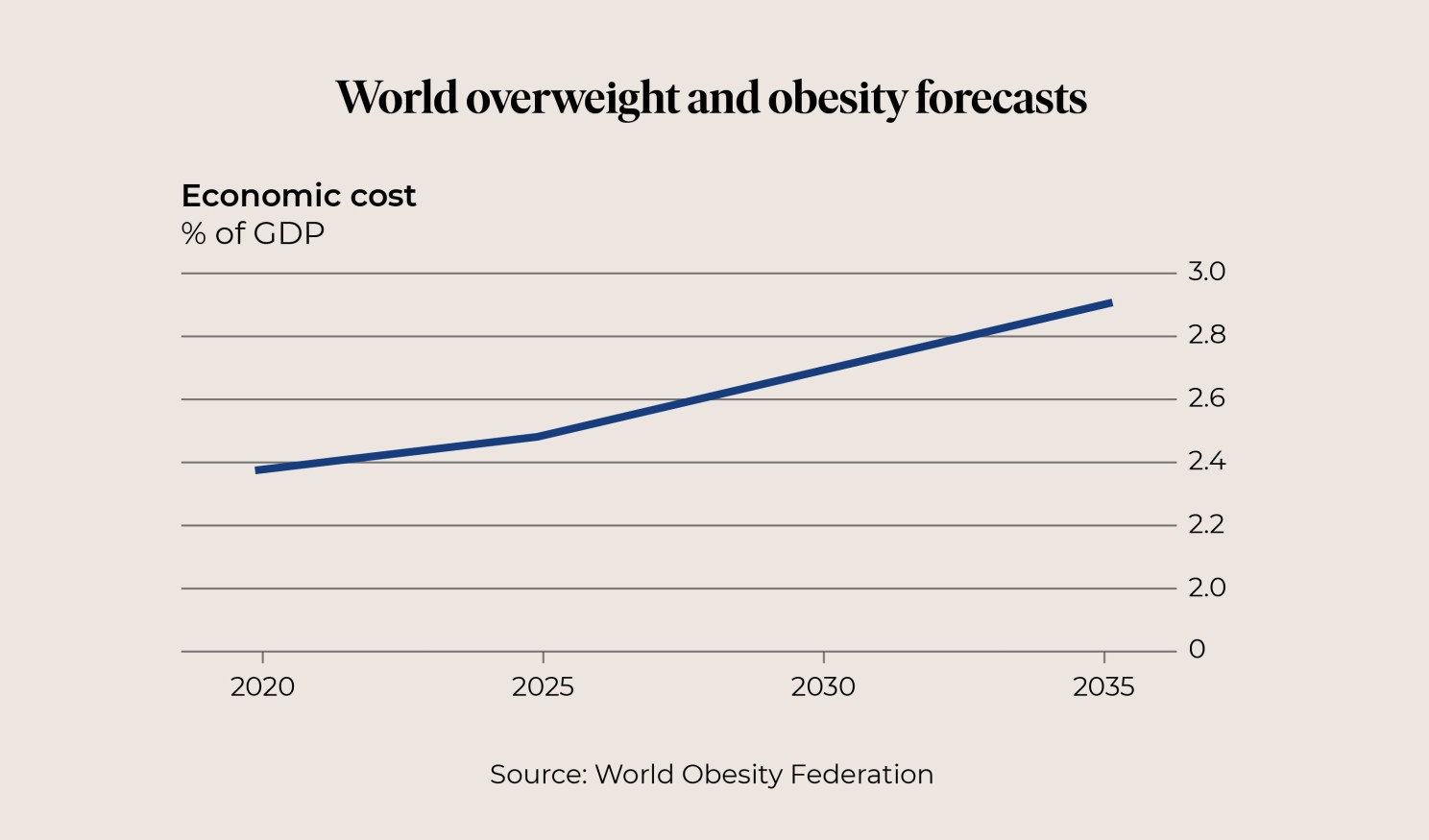
A recent report estimates the annual cost of humanity's bigger belly will hit $4 trillion in 2035.
That’s nearly 3% of global GDP in terms of both healthcare spending and of productivity lost to illness and premature deaths, the equivalent of another COVID-19 pandemic.
Every year.
So, it just seems common sense that any treatment that can reverse these numbers and improve the health of billions should be seriously considered.
Both the FDA in the United States and the NHS in the United Kingdom have already approved this new obesity therapy, although in the UK currently only for targeted populations.
As nations look at their growing healthcare costs, the long-term cost-benefits of obesity reducing drugs are likely to be given serious consideration.
Money saved from a reduction in obesity’s effects could be used to support other healthcare needs.
Like more and better paid nurses, more ambulances, more hospital beds and funding of new lifesaving cancer drugs.
However, with any new drug, comes risk.
Like most medication, Semaglutide can have side effects; these include nausea, stomach pain, vomiting and diarrhea.
Semaglutide too, also appears to increase the risk of a rare type of pancreatitis and there are unanswered questions over what effect it may have during or just before pregnancy.
So, who will it be available to, when and how much will it cost?
Unfunded, it’s not cheap. And once prescribed, it needs to be used for life, in the same way blood pressure medication needs to be used continually.
In Britain where the NHS has just approved its use, it’s priced at around NZ$150 per four injections when prescribed through Boot’s online doctor services. In the USA, monthly costs of $1,400 are touted.
There are reports that Elon Musk swears by it.
Cost, of course, is not a problem for him, Hollywood stars or the growing list of influencers singing its praises on TikTok.
For my money, it marks a significant development. It positions obesity as a health condition rather than the result of lack of self-control. A condition that can be treated by a new therapy which provides both individual and population benefits.
If obesity rates continue to rise, millions upon millions of people worldwide are likely to suffer debilitating and life-shortening health issues.
It therefore seems practical to propose that, should these types of drugs be proven safe and effective, they should be available to more than celebrities and billionaires, so ordinary people can benefit.
Because in many relatively high-income countries like New Zealand, obesity rates are higher for people with low incomes. They are also higher for our Pasifika and Māori communities.
It will therefore be interesting to see how the debate develops in New Zealand, where Pharmac is tasked with investing the nation’s pharmaceutical budget wisely to enhance wellbeing and deliver equitable health outcomes.
As usual I’d love to hear your thoughts or observations on this important issue, please share and comment on the post below or drop me an email at ceo@unimed.co.nz.
Nga mihi,
Louise.

